A generation ago, most people with multiple sclerosis could expect to rely on walkers and wheelchairs or be limited to their bed within 15 years of diagnosis. Today, UC San Francisco’s discoveries are keeping millions with MS healthier for longer – many disability-free. Now, the university is paving the way for an MS cure in our lifetimes.
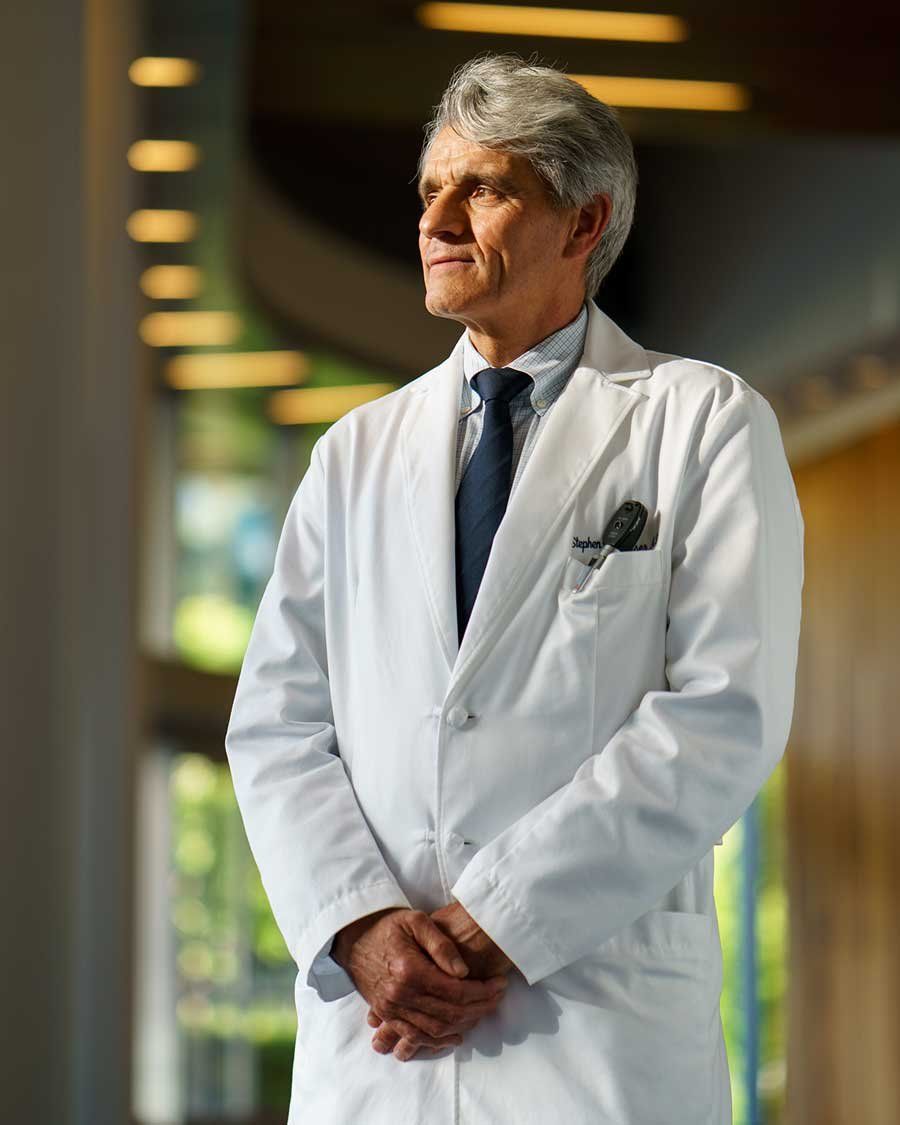
But the breakthrough almost didn’t happen. “Biologically implausible,” is what the National Institutes of Health’s rejection letter said. It was the late ’90s and UCSF Neurology Professor Stephen Hauser, MD, and team had applied for federal funding for the first clinical trial of the new medicine, rituximab, as a potential MS treatment.
The study wouldn’t just test a new drug, but a revolutionary new theory about MS’ inner workings. So outlandish was the idea that the largest public funder of scientific research said it couldn’t be done.
The rejection “hit like a ton of bricks,” Hauser remembered in his 2023 memoir, The Face Laughs While the Brain Cries. But if Hauser’s team proposed another trial, following conventional wisdom, the institutes assured him there was money.
The message was clear: “Just forget your last 15 years of work, kid, and do what we think.”

‘I decided right there that this would be my life’s work’
Two decades earlier as a young medical resident, Hauser treated 27-year-old Andrea. A recent Harvard Law graduate, Andrea was a rising star in President Jimmy Carter’s administration. Then, as sudden as a lightning strike, her behavior became erratic. By the time Hauser saw her, she was propped up in a hospital bed, the right side of her mouth drooping, saliva pooling at the corner.
“How are you,” he remembered asking her. Andrea tried to speak but her words came out garbled. A single tear rolled down her face.
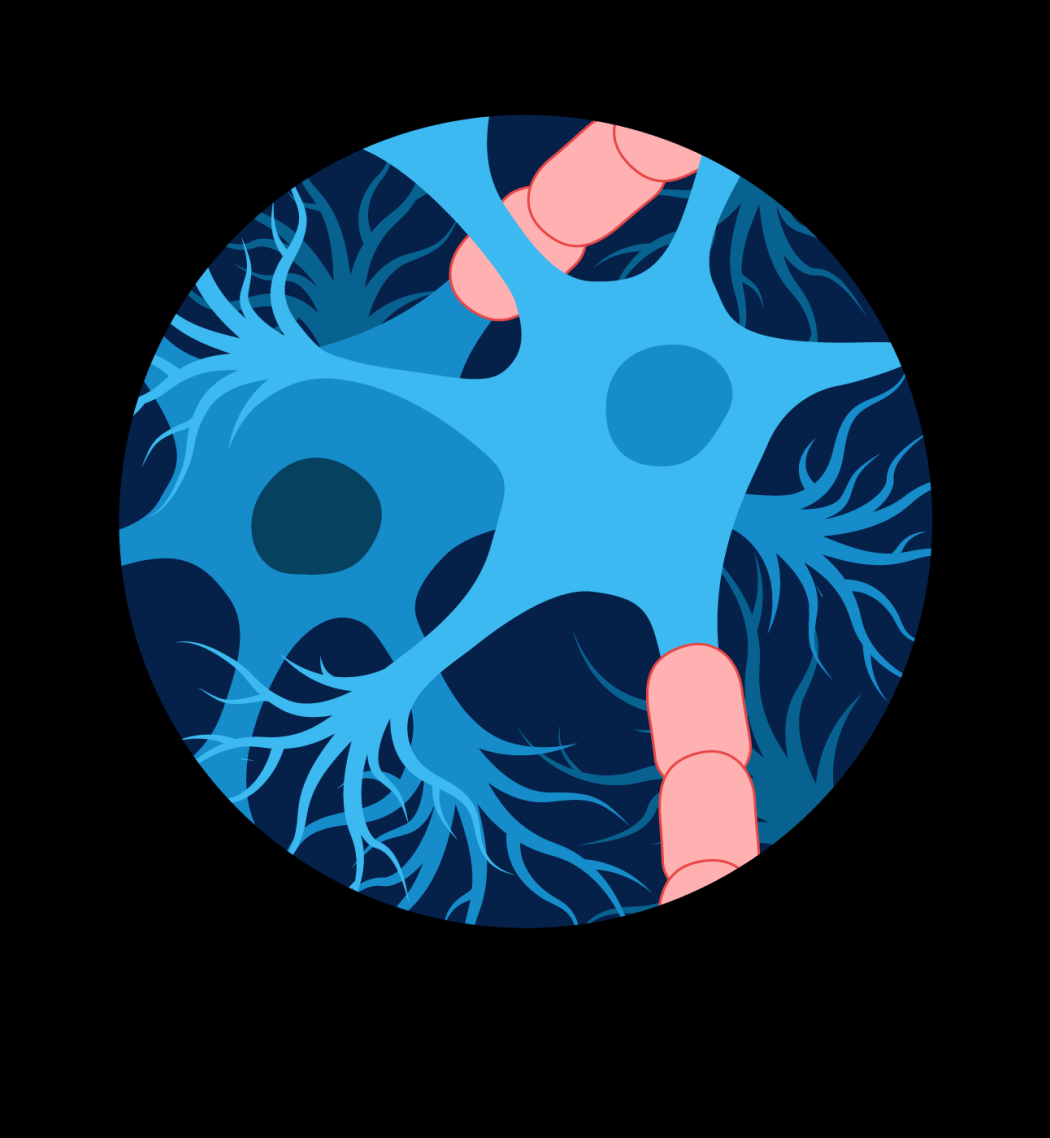
MS is a disease of the brain and immune system. Our brains contain a network of billions of neurons, nerve cells that send messages telling our mouth to speak, our legs to move and our lungs to breathe. Each neuron is wrapped in myelin, a protective coating like the plastic sheath around a copper electrical wire. But with MS, our immune system – which normally protects us against germs – mistakes myelin for a foreign invader. This case of mistaken identity prompts an all-out assault. The immune system attacks the myelin, short-circuiting our neurons like frayed power cords.
“Over time, the connections between nerves are lost, nerve cells die. MS robs people of basic functions we take for granted – vision, sensation, motor strength … and sometimes, as with Andrea, even the ability to speak, eat or breathe independently,” Hauser said.
With no effective treatment, there was nothing Hauser could do for Andrea. “I decided right there that this common, crippling disease of young adults would be my life’s work.”
‘I decided right there that this would be my life’s work’
Two decades earlier as a young medical resident, Hauser treated 27-year-old Andrea. A recent Harvard Law graduate, Andrea was a rising star in President Jimmy Carter’s administration. Then, as sudden as a lightning strike, her behavior became erratic. By the time Hauser saw her, she was propped up in a hospital bed, the right side of her mouth drooping, saliva pooling at the corner.
“How are you,” he remembered asking her. Andrea tried to speak but her words came out garbled. A single tear rolled down her face.
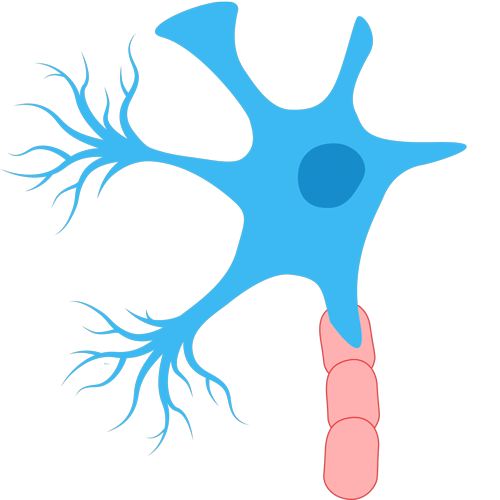
MS is a disease of the brain and immune system. Our brains contain a network of billions of neurons, nerve cells that send messages telling our mouth to speak, our legs to move and our lungs to breathe. Each neuron is wrapped in myelin, a protective coating like the plastic sheath around a copper electrical wire. But with MS, our immune system – which normally protects us against germs – mistakes myelin for a foreign invader. This case of mistaken identity prompts an all-out assault. The immune system attacks the myelin, short-circuiting our neurons like frayed power cords.
“Over time, the connections between nerves are lost, nerve cells die. MS robs people of basic functions we take for granted – vision, sensation, motor strength … and sometimes, as with Andrea, even the ability to speak, eat or breathe independently,” Hauser said.
With no effective treatment, there was nothing Hauser could do for Andrea. “I decided right there that this common, crippling disease of young adults would be my life’s work.”
Watch the story behind Stephen Hauser’s 40-year journey in MS research that lead to the drug that holds new hope for hundreds of thousands of patients living with the disease.
Ambush at the gates
For decades, doctors suspected that T-cells – a type of white blood cell that acts like the immune system’s detectives to identify intruders – were behind the myelin attacks. By the 1980s, Hauser had developed a means to test this theory, after gathering evidence that another immune soldier, B-cells, were the real culprits.
Our bodies are built to protect our brains and nervous system from infections, keeping them safe behind what doctors call the “blood-brain barrier” – a cellular city wall. Hauser proved that in MS, T-cells disrupted this barrier, opening the proverbial city gates, but it was B-cells and the proteins they produce that attacked nerve cells’ myelin coatings, short-circuiting the brain’s network of neurons.
Rituximab, which killed B-cells, had been too risky for federal funding but not for industry.
“The federal government has to rely on expert referees to guide funding decisions, and it’s very difficult to turn around entrenched ideas, even if there’s all sorts of wonderful biology behind the new idea,” said Hauser, explaining why he understood the NIH’s initial rejection. “And it’s important that the federal government not spend their resources funding new ideas that most experts feel are unlikely to succeed; this protects us all against the use of public funds to advance crackpot ideas.”
He adds: “The really high risk, high reward ideas have to be funded through philanthropy and industry.”
Pharmaceutical company Genentech, co-founded by UCSF professors, agreed to fund what would become a wildly successful trial of the drug as an MS treatment. Rituximab stopped the disease virtually in its tracks, changing the face of MS forever. The breakthrough led to the 2017 development of a second MS medicine, ocrelizumab and then a third, ofatumumab, in 2020, also pioneered by Hauser and his UCSF colleagues working closely with industry partners.
“Beautifully, this is a UCSF story but it also involves great colleagues at other centers across the globe, courageous industry leaders and fantastic philanthropists who believed in high-risk work at a time when traditional funding sources would never be able to support this research,” Hauser said. “And finally, without the thousands of patients who trusted in us and were courageous enough to volunteer for these clinical studies, this progress could never have been made.”
Lessons for Alzheimer’s, Parkinson’s and ALS
Today, this trio of drugs is the standard treatment for MS globally, allowing many people to escape the fate that befell Andrea decades ago.
“What’s most exciting to me is that these medicines have been associated with dramatic gains for patients,” Hauser said. “I am confident that people whose MS is just beginning can truly be optimistic about their prospects for a life free from disability – this is completely different from a generation ago.”
Today, clinical studies like those being conducted by the UCSF Weill Institute for Neurosciences, which Hauser directs, are investigating new ways to aggressively treat MS sooner with existing medications and new, more powerful versions. The Institute is also applying lessons learned from MS to develop treatments for degenerative brain disorders like Alzheimer’s and Parkinson’s, as well as ALS (amyotrophic lateral sclerosis).
Roadmap to repair myelin
And in the last decade, UCSF researchers have made incredible advances that could, one day, reverse MS symptoms or even treat the disease before it begins.
In 2013, physician-scientist Ari Green, MD, and neuroscientist Jonah Chan, PhD, made a startling discovery: The over-the-counter antihistamine clemastine repaired damaged myelin in laboratory tests. But could it work to heal the brain in people and turn back the clock on years of MS, they wondered? A decade later, they had their answer: Yes.
“Our study provided the first direct biologically validated imaging-based evidence of myelin repair induced by clemastine,” Green said on the heels of the 2023 discovery. Unfortunately, at high doses the drug store medication has too many side effects to be used as an MS treatment. Still, Green and Chan’s research proves repairing myelin is possible. “It’s set the standard for future research into remyelinating therapies.”
A few months after Green and Chan’s discovery, UCSF Neurology Professor Sergio Baranzini, PhD, and an international team provided the world’s first clues to why, 10 years after a diagnosis, some MS patients are in wheelchairs while others are running marathons.
The 2023 study showed people who inherited a specific genetic variant from both parents, were likely to need a walking aid about four years sooner than those without. This genetic variation sits between two genes that help to repair damaged cells and control viral infections, but it had never been linked to MS.
This newfound understanding of the genetic markers of MS could lead to a new era in precision medicine for MS treatments.
“Our findings suggest that resilience and repair in the nervous system determine the course of MS progression, and that we should focus on these parts of human biology for better therapies,” explained Adil Harroud, a former postdoctoral researcher in the Baranzini Lab and co-lead author of the study.


‘All of the pieces are in place to soon reach the finish line – a cure’
With new treatments on the horizon, doctors are closer than ever to treating MS before symptoms begin.
In just the last year, Hauser, Green, Chan and Baranzini have joined UCSF professors Michael Wilson, MD, and Joe DeRisi, PhD, and others in revealing new clues into who will develop MS . By comparing hundreds of blood samples from armed forces veterans who went onto develop MS after enlisting to those who remained MS-free, UCSF researcher Colin Zamecnik, PhD, and these researchers found that in some patients markers of MS might be present in the bloodstream years before symptoms appear.


The research is still in its early phases and cannot be used to diagnose patients. Still, it may pave the way to treating the disease almost before it begins.
“Over the last few decades, there’s been a move in the field to treat MS earlier and more aggressively with newer more potent therapies,” said UCSF neurologist Michael Wilson, MD, earlier this year. “A diagnostic result like this makes such early intervention more likely, giving patients hope for a better life.”
Hauser, meanwhile, is hopeful that the world is on the cusp of a new era in MS.
“I think we can, in the next few years, completely suppress the disease in most people, if the proverbial tea leaves continue to point in the direction that they do today,” he said. And a cure for MS could be close behind.
“The battle is not yet won, but all of the pieces are in place to soon reach the finish line – a cure for MS.”
Roadmap to repair myelin
And in the last decade, UCSF researchers have made incredible advances that could, one day, reverse MS symptoms or even treat the disease before it begins.
In 2013, physician-scientist Ari Green, MD, and neuroscientist Jonah Chan, PhD, made a startling discovery: The over-the-counter antihistamine clemastine repaired damaged myelin in laboratory tests. But could it work to heal the brain in people and turn back the clock on years of MS, they wondered? A decade later, they had their answer: Yes.
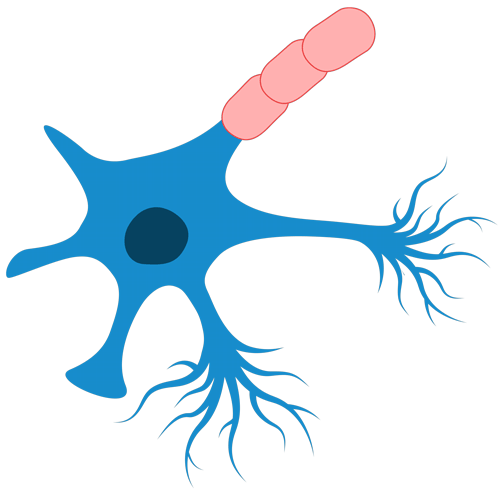
“Our study provided the first direct biologically validated imaging-based evidence of myelin repair induced by clemastine,” Green said on the heels of the 2023 discovery. Unfortunately, at high doses the drug store medication has too many side effects to be used as an MS treatment. Still, Green and Chan’s research proves repairing myelin is possible. “It’s set the standard for future research into remyelinating therapies.”
A few months after Green and Chan’s discovery, UCSF Neurology Professor Sergio Baranzini, PhD, and an international team provided the world’s first clues to why, 10 years after a diagnosis, some MS patients are in wheelchairs while others are running marathons.
The 2023 study showed people who inherited a specific genetic variant from both parents, were likely to need a walking aid about four years sooner than those without. This genetic variation sits between two genes that help to repair damaged cells and control viral infections, but it had never been linked to MS.
This newfound understanding of the genetic markers of MS could lead to a new era in precision medicine for MS treatments.
“Our findings suggest that resilience and repair in the nervous system determine the course of MS progression, and that we should focus on these parts of human biology for better therapies,” explained Adil Harroud, a former postdoctoral researcher in the Baranzini Lab and co-lead author of the study.


‘All of the pieces are in place to soon reach the finish line – a cure’
With new treatments on the horizon, doctors are closer than ever to treating MS before symptoms begin.
In just the last year, Hauser, Green, Chan and Baranzini have joined UCSF professors Michael Wilson, MD, and Joe DeRisi, PhD, and others in revealing new clues into who will develop MS . By comparing hundreds of blood samples from armed forces veterans who went onto develop MS after enlisting to those who remained MS-free, UCSF researcher Colin Zamecnik, PhD, and these researchers found that in some patients markers of MS might be present in the bloodstream years before symptoms appear.


The research is still in its early phases and cannot be used to diagnose patients. Still, it may pave the way to treating the disease almost before it begins.
“Over the last few decades, there’s been a move in the field to treat MS earlier and more aggressively with newer more potent therapies,” said UCSF neurologist Michael Wilson, MD, earlier this year. “A diagnostic result like this makes such early intervention more likely, giving patients hope for a better life.”
Hauser, meanwhile, is hopeful that the world is on the cusp of a new era in MS.
“I think we can, in the next few years, completely suppress the disease in most people, if the proverbial tea leaves continue to point in the direction that they do today,” he said. And a cure for MS could be close behind.
“The battle is not yet won, but all of the pieces are in place to soon reach the finish line – a cure for MS.”
MS Milestones Through the Decades
-
2006
UCSF’s Stephen Hauser, MD, reveals the first research results showing that the cancer drug rituximab works to reduce inflammation in the brain caused by MS. -
2008
Rituximab becomes widely used globally as the first effective treatment for MS.
-
2017
FDA approves ocrelizumab to treat MS. The drug’s approval further validates Hauser’s theory about the role of B-cells in MS disease and treatment.
-
2020
FDA approves another B-cell targeting drug, ofatumumab, to treat relapsing forms of MS. -
February 2023
After a decade of study, UCSF’s Jonah Chan, PhD, and Ari Green, MD, prove the over-the-counter allergy drug, clemastine, can repair neurons’ myelin coating in the brain damaged by MS, opening a door to possible future research. -
June 2023
UCSF’s Sergio Baranzini, PhD, leads an international team to discover that, in some patients, faster MS progression is tied to a particular genetic variant inherited from both parents. This new understanding could allow scientists to begin developing treatments that target the nervous system. -
2024
Hauser, Green, Chan and Baranzini join UCSF’s Michael Wilson, MD, and Joe DeRisi, PhD, and others to discover that, for some, markers for MS are visible years before the first symptoms appear.